Anatomy of the Heart
- Home
- Anatomy of the Heart
Anatomy of the Heart
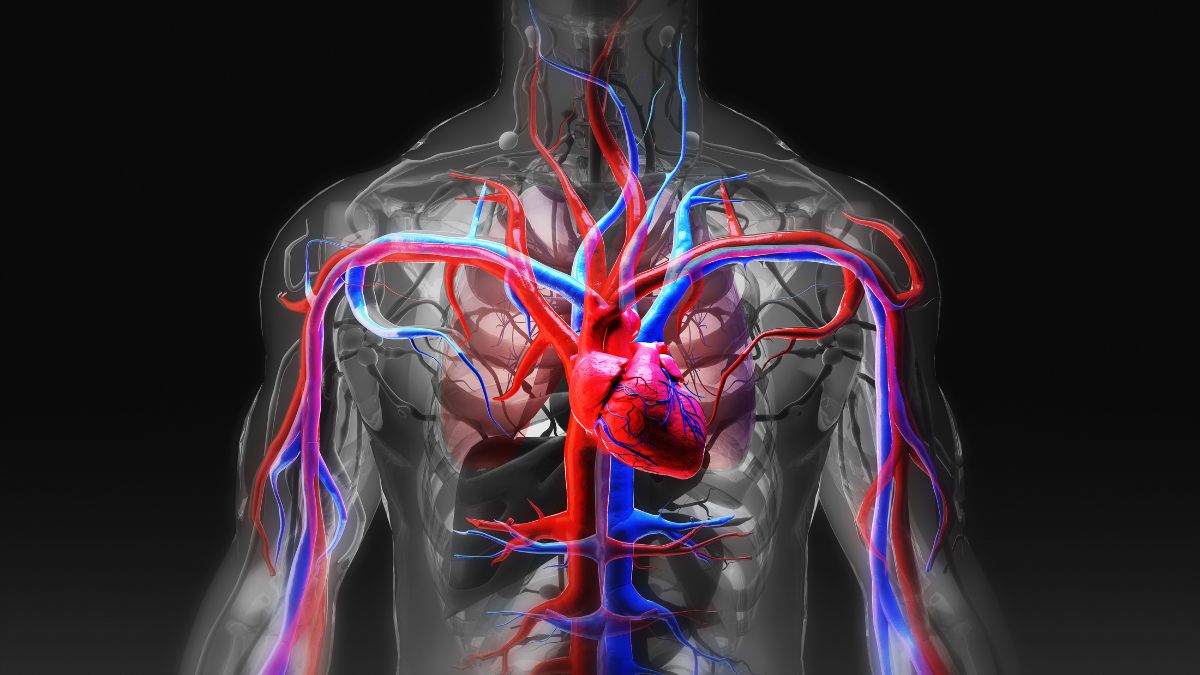
The human heart, a symbol of love and the essence of vitality, serves as the central orchestrator of our circulatory system. This tireless organ, tucked away within the chest, sustains life by relentlessly pumping blood throughout our bodies. In this comprehensive examination, we delve into the mesmerizing intricacies of the heart’s anatomy, uncovering the secrets of its structure, and gaining a profound understanding of its critical role in sustaining life.
Location and Position of the Heart
Our journey into the heart’s anatomy begins with its precise location. The heart is strategically positioned within the thoracic cavity, slightly left of the body’s midline. Nestled between the two lungs and enveloped by the protective ribcage, its placement is nothing short of ingenious. This central location allows the heart to efficiently pump oxygenated blood to the body’s tissues while receiving deoxygenated blood from various tissues.
This precise location is not arbitrary; it’s central to its role as the body’s circulatory powerhouse. Placing the heart in the chest offers protection from external harm while facilitating its critical functions.
The Protective Pericardium
To safeguard this vital organ, nature has bestowed it with a protective layer known as the pericardium. The pericardium serves as the heart’s guardian, offering both structural support and lubrication for its seamless movements.
Fibrous Pericardium: The outer layer of the pericardium, known as the fibrous pericardium, is a tough, protective coat that anchors the heart in place within the chest. It prevents overstretching and helps maintain the heart’s position.
Serous Pericardium: Beneath the fibrous pericardium lies the serous pericardium, which secretes a lubricating fluid. This fluid allows the layers of the pericardium to glide smoothly over each other as the heart contracts and relaxes. It is akin to the heart’s personal lubrication system, reducing friction and facilitating its rhythmic movements.
Layers of the Heart Wall
Having uncovered the heart’s protective layers, we now venture deeper into its core to examine its intrinsic structure:
Epicardium: The outermost layer of the heart is the epicardium, also known as the visceral pericardium. Composed of connective tissue and a layer of fat, it serves as a protective covering for the heart. Beyond protection, the epicardium also plays a role in secreting the lubricating fluid found in the pericardial cavity.
Myocardium: The myocardium, situated beneath the epicardium, is the heart’s muscular middle layer. This is where the magic happens. Composed primarily of cardiac muscle tissue, the myocardium is responsible for the heart’s rhythmic contractions. It contracts vigorously to pump blood throughout the circulatory system, with the left ventricle being the most muscular due to its role in pumping oxygenated blood to the entire body.
Endocardium: As we delve deeper, we encounter the endocardium, the innermost layer of the heart wall. Comprising a thin layer of endothelial tissue, the endocardium forms the lining of the heart’s chambers and covers the heart valves. This smooth inner lining ensures that blood flows easily and without friction as it courses through the heart.
The Four Chambers of the Heart
Having unveiled the heart’s layers, our journey takes us into its interior, where we encounter its four chambers, each with a unique role in the circulatory process:
Atria:
Right Atrium: Starting on the right side of the heart, we encounter the right atrium. This chamber serves as the receiving room for deoxygenated blood returning from the body’s various tissues. Two major veins, the superior vena cava (which collects blood from the upper body) and the inferior vena cava (which collects blood from the lower body), deliver this deoxygenated blood to the right atrium.
Left Atrium: Across from the right atrium lies the left atrium. This chamber’s role differs from the right atrium. It serves as the heart’s gateway for freshly oxygenated blood returning from the lungs, thanks to the pulmonary veins. The left atrium prepares to send this oxygen-rich blood onward through the heart’s chambers.
Ventricles:
Right Ventricle: Below the right atrium, we encounter the right ventricle. This chamber is tasked with pumping deoxygenated blood to the lungs, where it will undergo oxygenation. As the right ventricle contracts, it propels blood through the pulmonary valve and into the pulmonary artery, setting the stage for the blood’s journey to the lungs.
Left Ventricle: Nestled beneath the left atrium is the left ventricle, often celebrated as the heart’s powerhouse. Distinguished by its muscular walls, significantly thicker than those of the right ventricle, the left ventricle is responsible for pumping oxygen-rich blood to nourish the entire body. When the left ventricle contracts, it propels blood through the aortic valve and into the aorta, the body’s largest artery, initiating the vital mission of delivering oxygen and nutrients to cells across the body.
Coronary Arteries
The heart has its own circulatory system, known as coronary circulation, which ensures that the heart muscle itself receives the oxygen and nutrients it needs to function effectively. Two primary coronary arteries play a pivotal role:
Right Coronary Artery (RCA): The right coronary artery primarily supplies the right atrium and right ventricle with oxygenated blood. It follows a path along the surface of the heart, branching into smaller arteries that penetrate the heart muscle.
Left Coronary Artery (LCA): The left coronary artery, the larger of the two, branches into two major arteries:
- Left Anterior Descending (LAD) Artery: It travels down the anterior surface of the heart, supplying blood to the anterior ventricles and a portion of the interventricular septum.
- Left Circumflex Artery (LCx): This artery encircles the heart, nourishing the left atrium and a portion of the left ventricle.
These coronary arteries, through their branches, form an intricate network that ensures the heart muscle receives a continuous supply of oxygen and nutrients. Without this system, the heart’s own cells would suffer, potentially leading to ischemia (lack of oxygen) and damage to the heart muscle.
Aorta and Pulmonary Artery
Beyond supplying itself, the heart’s primary role is to pump blood to the rest of the body. Two major vessels facilitate this:
Aorta: The aorta, originating from the left ventricle, is the body’s largest artery. It carries oxygen-rich blood away from the heart, branching into smaller arteries that distribute blood to various organs and tissues throughout the body.
Pulmonary Artery: In contrast, the pulmonary artery, originating from the right ventricle, carries deoxygenated blood to the lungs for oxygenation. It’s a rare instance where an artery carries deoxygenated blood. After the blood is oxygenated in the lungs, it returns to the heart via the pulmonary veins to continue its journey.
The Intricacies of Heart Function
Now that we’ve mapped out the heart’s components, it’s time to understand how they work together to fulfill the heart’s primary function: pumping blood throughout the body. This process involves an intricate series of events known as the cardiac cycle.
Blood Flow: It all begins with blood returning to the heart. Deoxygenated blood flows into the right atrium from the body through the superior and inferior vena cavae.
Atria Contraction: The right atrium contracts, squeezing blood through the open tricuspid valve into the right ventricle.
Ventricular Contraction (Right Ventricle): The right ventricle contracts forcefully, pushing blood through the pulmonary valve into the pulmonary artery. This deoxygenated blood is now en route to the lungs for oxygenation.
Lung Oxygenation: In the lungs, oxygen exchange occurs. Carbon dioxide is released from the blood, and oxygen is absorbed. Blood becomes oxygen-rich.
Return to the Heart: Oxygenated blood returns to the heart, specifically to the left atrium, through the pulmonary veins. The left atrium contracts, driving blood through the open bicuspid valve into the left ventricle.
Ventricular Contraction (Left Ventricle): The left ventricle, the heart’s powerhouse, contracts vigorously. It expels oxygen-rich blood through the aortic valve into the aorta, ready to nourish the body’s cells.
Distribution to the Body: The aorta and its branches carry oxygenated blood to all corners of the body, ensuring that every cell receives the vital oxygen and nutrients it needs to function.
This cardiac cycle repeats continuously, maintaining the body’s oxygen supply and supporting metabolic processes.
The Heart's Development: From Conception to Birth
The journey of the heart begins long before birth, during embryonic development. Understanding the stages of heart development is crucial for comprehending congenital heart defects and appreciating the heart’s complexity.
Embryonic development unfolds as a sequence of highly orchestrated events. The heart begins as a simple tube and evolves into a complex, four-chambered organ. Key milestones in heart development include:
Formation of the Heart Tube: Around the third week of gestation, the heart tube forms from a pair of primitive tubes. These tubes fuse and give rise to the single primitive heart tube.
Partitioning of the Heart: Over the next several weeks, the heart tube undergoes a series of partitions, or divisions, that eventually create four distinct chambers: two atria and two ventricles.
Development of Heart Valves: As the heart takes shape, valves begin to form. These valves are crucial for directing blood flow and ensuring that it moves in the right direction.
Connection to the Circulatory System: As the heart develops, it connects to the circulatory system, initially bypassing the lungs. Shunts like the foramen ovale and ductus arteriosus allow blood to flow efficiently in the oxygen-rich environment of the womb.
By the time of birth, the heart is fully formed and equipped to function in the external world. However, the transition from fetal to postnatal circulation involves closing these shunts and adapting to the demands of oxygenating blood in the lungs.
Heart Health: A Lifelong Pursuit
Maintaining heart health is a lifelong endeavor that begins with understanding the factors that contribute to cardiovascular well-being. Lifestyle choices, genetics, and environmental factors all play pivotal roles in determining heart health.
Lifestyle Factors and Heart Health
Diet: A heart-healthy diet emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting saturated and trans fats, sodium, and added sugars. This dietary pattern can help prevent conditions like coronary artery disease and hypertension.
Physical Activity: Regular exercise strengthens the heart and improves circulation. Engaging in aerobic activities, such as brisk walking, swimming, or cycling, can promote cardiovascular health.
Weight Management: Maintaining a healthy weight reduces the risk of heart disease. Losing excess weight through a balanced diet and regular physical activity can have a significant positive impact on heart health.
Stress Management: Chronic stress can contribute to heart disease. Stress-reduction techniques, such as meditation, deep breathing exercises, and yoga, can help manage stress and promote heart health.
Smoking Cessation: Smoking is a major risk factor for heart disease. Quitting smoking can lead to immediate and long-term cardiovascular benefits.
Moderate Alcohol Consumption: While excessive alcohol consumption is detrimental to heart health, moderate alcohol intake, especially red wine, in the context of a balanced diet, may have certain cardiovascular benefits. However, it’s essential to consult with a healthcare provider regarding alcohol consumption.
Genetics and Heart Health
Genetics also plays a role in heart health. Some individuals may be genetically predisposed to certain heart conditions, such as familial hypercholesterolemia or genetic arrhythmias. Understanding one’s family history and undergoing genetic testing, when appropriate, can help identify genetic risk factors and inform preventive measures.
Environmental Factors and Heart Health
Genetics also plays a role in heart health. Some individuals may be genetically predisposed to certain heart conditions, such as familial hypercholesterolemia or genetic arrhythmias. Understanding one’s family history and undergoing genetic testing, when appropriate, can help identify genetic risk factors and inform preventive measures.
Conclusion
The human heart, with its intricate anatomy and relentless functionality, stands as a testament to the remarkable complexity of the human body. It beats unceasingly, driving life’s essence through our veins, providing the oxygen and nutrients our cells require to thrive.
This exploration of the heart’s anatomy and function has unveiled the mysteries of this vital organ. It empowers us to make informed choices to maintain its health, comprehend the challenges posed by heart conditions, and appreciate the remarkable progress made in cardiology.
As we continue to unravel the enigma of the human heart through research and innovation, we glimpse a future where heart disease may be conquered, extending the gift of life and vitality to countless individuals worldwide. The heart’s enduring legacy is one of resilience, strength, and unwavering commitment to life itself.
Surgeries We Offer
- Beating Heart Bypass Surgery
- Beating Heart Bypass Surgery In Acute MI
- Beating Heart Bypass Surgery In Poor LV Function
- Endoscopic Vein Harvesting
- Valve Replacements Single or Double
- Combined CABG & Valve Replacements
- Repair of Congenital Heart Defects
- Closed Heart Surgery
- Pericardiectomy
- Peripheral Vascular Surgeries
- Surgery Of Aortic Dissection
- Conventional Bypass Surgery On Pump
Emergency Cases
Please feel welcome to contact our friendly reception staff with any general or medical enquiry call us.
